Evidence‑Based Care for Children’s Breathing, Sleep, and Growth

At MyoWay, our therapy is grounded in scientific evidence. Pediatric myofunctional therapy has been evaluated in clinical studies and case reports that demonstrate meaningful outcomes in airway development, sleep quality, and functional muscle retraining.
Our Science and Research page is a curated resource designed for parents and healthcare professionals who want to understand the clinical foundations of myofunctional therapy. You’ll find downloadable PDFs covering:
Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management
Sleep Difficulties and Symptoms of Attention-deficit Hyperactivity Disorder in Children with Mouth Breathing
The Effect of Breathing Exercises on the Nocturnal Enuresis in the Children with the Sleep-Disordered Breathing
Relationship Between Obstructive Sleep Apnea and Enuresis in Children: Current Perspectives and Beyond
Probable Sleep Bruxism in Children and its Relationship with Harmful Oral Habits, Type of Crossbite and Oral Breathing
The Link between Sleep Bruxism, Sleep Disordered Breathing and Temporomandibular Disorders
Investigation on the Effect of Oral Breathing on Cognitive Activity Using Functional Brain Imaging
Application of functional orthodontic appliances to treatment of “mandibular retrusion syndrome”
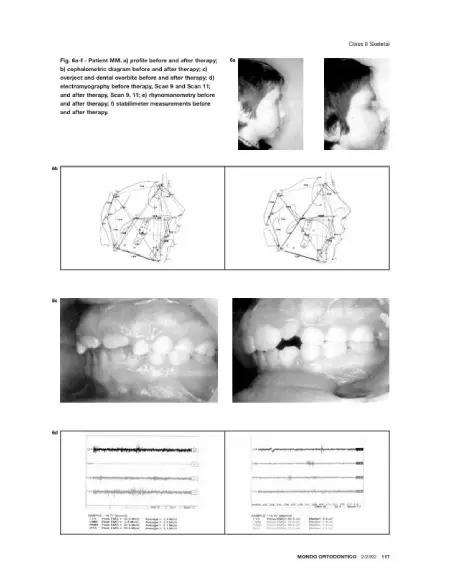
Non-invasive 3d facial analysis and surface electromyography during functional Pre orthodontic therapy: A preliminary report

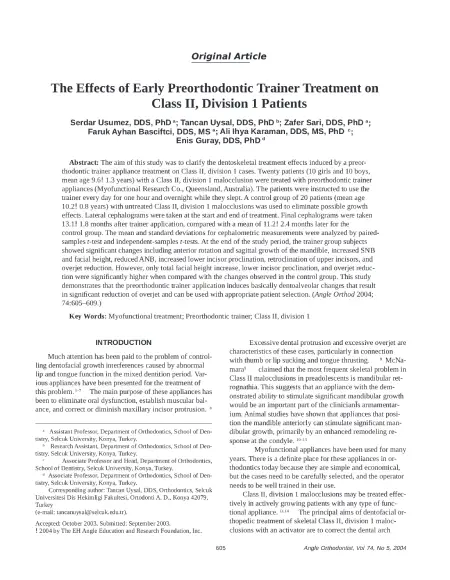
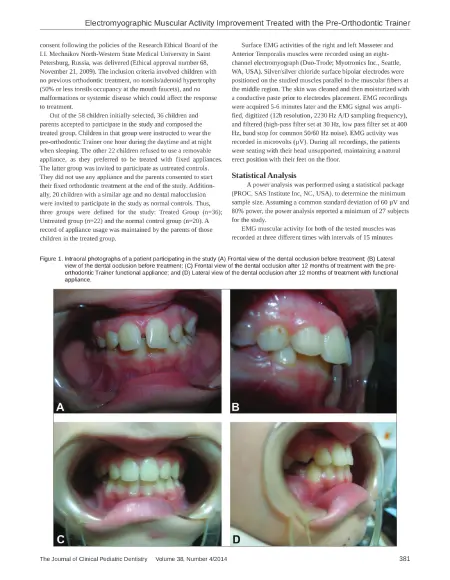
Electromyographic Muscular Activity Improvement in Class II Patients Treated with the Pre-Orthodontic Trainer
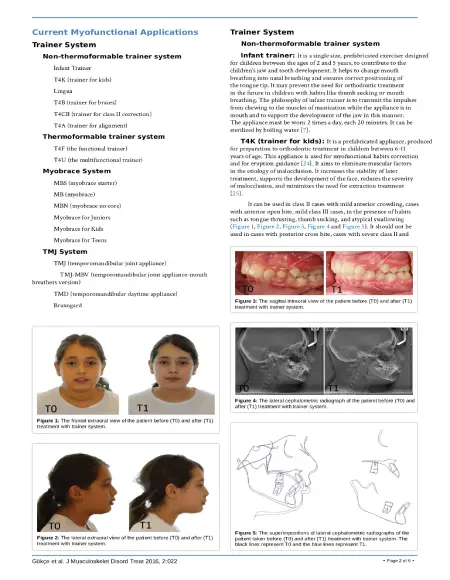
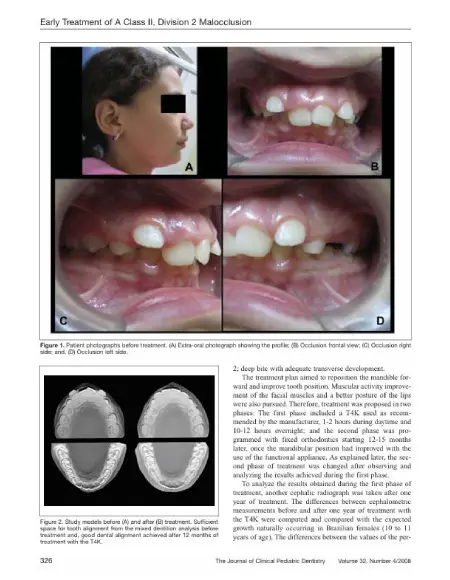
Early Treatment of a Class II, Division 2 Malocclusion with the Trainer for Kids (T4K) : A Case Report
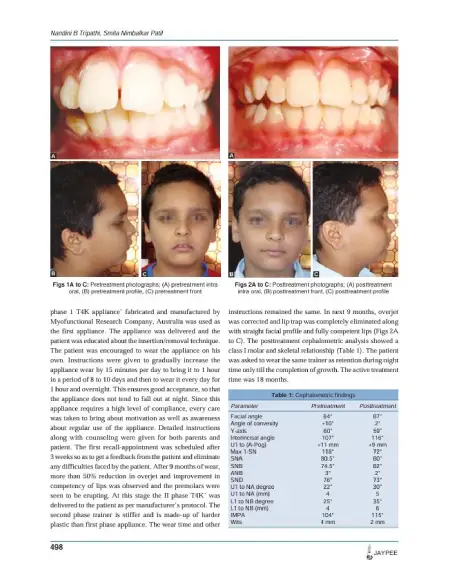
Treatment of Class II Division 1 Malocclusion with Myofunctional Trainer System in Early Mixed Dentition Period
A Systematic Review of Oral Myofunctional Therapy for Future Treatment in Pediatric Obstructive Sleep Apnea
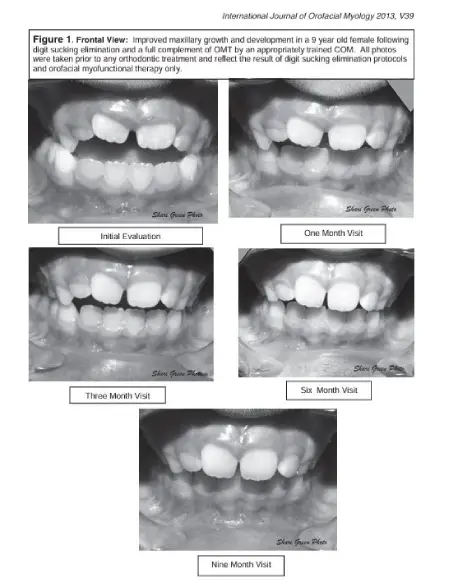
Improved Maxillary Growth and Development Following Digit Sucking Elimination and Orofacial Myofunctional Therapy
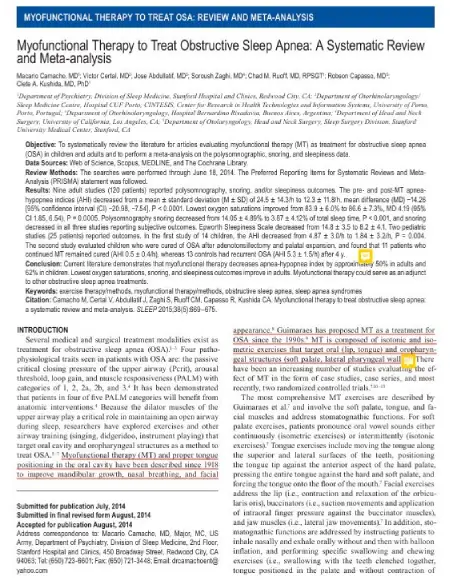
Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-analysis
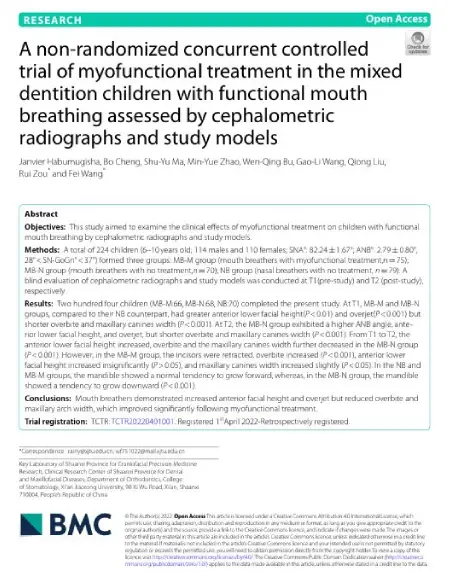
A non-randomized concurrent controlled trial of myofunctional treatment in the mixed dentition children with functional mouth breathing assessed
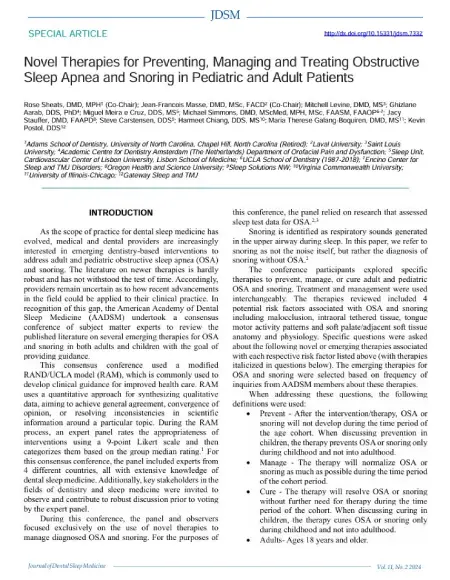
Novel Therapies for Preventing, Managing and Treating Obstructive Sleep Apnea and Snoring in Pediatric and Adult Patients
Orofacial Myofunctional Therapy: Investigating a Novel Therapeutic Approach for Pediatric Obstructive Sleep Apnea in Children

Orofacial myofunctional therapy with children ages 0-4 and Orofacial myofunctional therapy with children ages 0-4 and individuals with special needs
The Effects of Orofacial Myofunctional Therapy on Children with OSAHS’s Craniomaxillo facial Growth: A Systematic Review
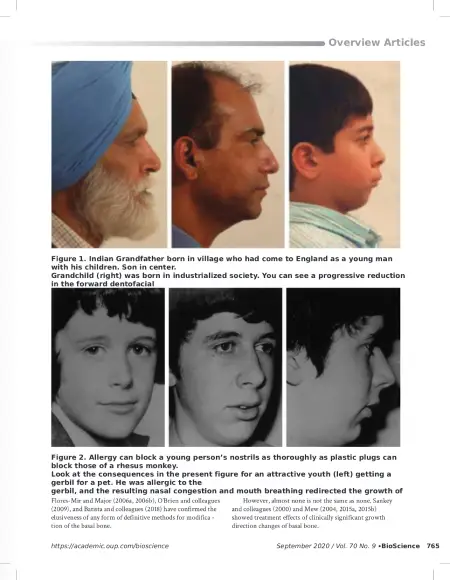
Establishment of nasal breathing should be the ultimate goal to secure adequate craniofacial and airway development in children
Effects of orofacial myofunctional therapy on masticatory function in individuals submitted to orthognathic surgery

Lingual and Maxillary Labial Frenuloplasty with Myofunctional Therapy as a Treatment for Mouth Breathing and Snoring

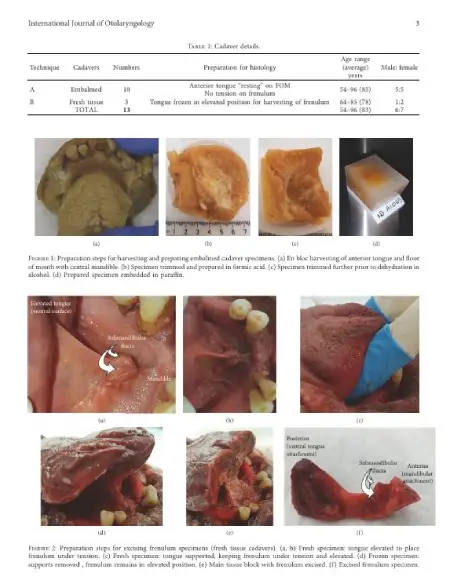
Understanding the Lingual Frenulum: Histological Structure, Tissue Composition, and Implications for Tongue Tie Surgery
Each document includes summaries, key findings, and practical insights you can discuss with your child’s care team. These resources help clarify how early muscle and airway support translates into improved outcomes in sleep, behavior, academic performance, and long‑term oral health.
By making research accessible, we empower families and professionals to make informed decisions that support the whole child.
Download, review, and share these resources — and contact us if you’d like help interpreting what the science means for your child.

Easy to do programs. Life-changing results.
Appliance guided therapy fits effortlessly into your child’s day. No pain. No stress. Just healthier breathing, better sleep, and lasting growth from the inside out. Click the button below, take the quiz and find out if your child is at risk.
Contact Our Team
Have a question? Send us a message and we’ll get back to you soon.